As if manufacturing of investigational medicinal products (IMPs) weren’t challenging enough already, the appropriate storage and distribution of sensitive biological products can be an adventurous journey itself — especially if not carefully planned and managed. No one solution fits all situations. Many things must be evaluated during planning stages. For example, what is more important: time to delivery or quality of transport and product integrity until drug can be administered to a patient?
It is important to understand key storage and distribution strategies such as central depots, direct-to-site shipments, and mixed alternatives that combine central and local depots. There is no one-size-fits-all solution. Therefore, it is important to evaluate the pros and cons of each option and identify the optimal individual study approach for your product. Storage typically does not end at a depot, so you must ensure that materials are stored safely at clinical sites and even with patients who are participating in clinical trials.
A holistic view of storage, distribution, and handling of deviations is essential for optimizing costs and ensuring product safety. Equally important is a distribution plan that reflects product stability and requirements of all countries involved. This is often the work of a contract manufacturing organization (CMO) and/or contract research organization (CRO), but as with all outsourced work, the results are ultimately the responsibility of a drug product’s sponsor company. Both sides of a contract relationship need to understand logistics.
Once, many clinical-trial–related distribution services were outsourced to CMOs. This was mainly to reduce total clinical supply chain cost. CMOs provided several benefits, including innovative packaging solutions and optimized product storage at their facilities. Over the past couple of years, however, we have seen a trend toward some distribution and manufacturing services being outsourced to CMOs and CROs in hybrid solutions. This is primarily due to CROs’ direct access to clinical sites and patients. Also, with CROs’ local legal entities already used for drug import, they can distribute effectively to local depots.
Defining a Clinical Trial Material Supply Chain Strategy
An annual PAREXEL clinical logistics industry survey of biopharmaceutical R&D supply chain leaders, conducted by ISR in fall 2013, identified the top three risks as product integrity, concern over supply chain disruptions, and need to meet timelines (1). Typically during the planning phase, project leaders need to clarify essential questions to prepare for successful storage and distribution of all clinical-trial materials at all times.
Certain parameters must be identified early to allow for planning a high-quality storage and distribution strategy. These should include the total number of investigational sites and patients; planned geographical distribution of sites and patients; product stability data and shelf life; available product quantities; frequency of administration; storage conditions (e.g., controlled ambient 15–25 °C); controlled or uncontrolled substance status; cost of drugs; and study length and planned enrollments. Sophisticated forecasting and software-aided simulations can help supply chain managers assess some key questions, including the quantity of medication required, minimum requirements for study launch, the best size and types of medication packs to produce, and the choice of central/local depots for efficient IMP use and supply.
For example, if (as for many recombinant biologics) product manufacturing is highly cost intensive and the drug is temperature sensitive with a short shelf life, then its supply chain solution may differ from that of a temperature-sensitive drug that is less expensive to produce (e.g., a vaccine). In the former case, the best strategy would be frequent shipments from a depot to the site; in the latter case, a much higher overage of products could be manufactured and higher quantities distributed to sites per shipment.
Geographical distribution also requires significant up-front planning. For example, treatment-naïve patient populations in emerging drug markets are considered to be attractive for trial recruitment. But it may take longer for trial approval by local authorities in some countries, and the local infrastructure for storage and distribution can be challenging. Furthermore, exporting/importing a drug might require specific customs processes and additional tax payments, which can drastically increase supply chain costs. Thus it is essential to work as closely as possible with local clinical teams to balance faster recruitment of patients and minimize total expected project cost.
| GDP Requirements Correct distribution of medicinal product relies on many requirements relating to facility/premises, equipment, documentation, operations, operational qualification, storage, and order fulfillment and export (2).Premises Requirements: The facility operates a proper cleaning and maintenance program and implements temperature and environmental controls (with suitable equipment and procedures in place to check and monitor the environment). Initial temperature mapping precedes installation of monitoring equipment.Equipment Requirements: Equipment and instrumentation is designed, located, and maintained to a standard that suits its intended purpose. Monitoring is calibrated at defined intervals based on risk and reliability assessments, including alarms when excursions from predefined storage conditions occur. Repair, maintenance, and calibration exercises do not impair medicinal products. Computer system validation ensures the ability of such systems to achieve desired results accurately and consistently. The scope of qualification and validation efforts must be determined to include installation, operational, and performance qualification (IQ, OQ, and PQ).Documentation Requirements: Whether in paper or electronic form, all written procedures, instructions, contracts, records, and data must exhibit a longevity of at least five years. Each record should include at least the product name; date; quantity received, supplied, or brokered; name and address of supplier(s); and batch number.Operational Requirements: A medicinal product’s identity must not be lost, and it must be distributed in accordance with information on its outer packaging. All medicinal products distributed in the European Union must be released by a qualified person (QP) in accordance with Annex 13 of the GDP guidelines (2). Qualification of suppliers should be controlled by documented procedures, including verifying that a supplier complies with GDP principles and guidelines. Qualification Requirements: Customer qualification ensures that holders of wholesale distribution authorization are qualified to do so. Groups in receipt of medicinal product must ensure that arriving consignments are correct. Medicinal products requiring special storage or security should be prioritized. Storage Requirements: According to storage conditions, all products must be stored separately from others that could alter their content. Breakage, spillage, and contamination must be prevented. Material approaching or beyond expiry dates should be withdrawn from available inventories, with obsolete goods appropriately identified and destroyed or removed from inventory. Records must be maintained. Order Fulfillment and Export Requirements: Controls must be in place. Documents such as bills of materials and delivery notes should state pertinent information (batch number, product, protocol, consignee, quantity, safety features, and so on). Complaints must be recorded with all details and associated corrective and preventive actions (CAPAs) should be established. Returns must be handled according to written procedures and conducted in accordance with national law. Should falsified medicinal products be discovered, the company must inform a competent authority of such materials suspected in accordance with written procedures. And companies should be able to initiate recalls promptly and handled them in accordance with written procedures. |
Ensuring Quality: Knowing Your Partners
In addition to planning ahead, an essential quality of a successful clinical supply chain is developing close relationships with reliable business partners. In the past, single projects were outsourced to CMOs and CROs; however, over the recent five or so years, many large biopharmaceutical companies engaged in strategic partnerships with their core suppliers. Meanwhile, CMOs and CROs began strengthening their relationships with core suppliers, such as special couriers and frequently used local depot providers. One key advantage of strategic, long-term partnerships is a constantly growing learning curve for both partners. This helps streamline processes and eliminate unnecessary steps along the journey of a drug, increasing clinical supply chain visibility along the way while reducing costs and improving quality.
Each and every supplier who participates in storing and distributing IMPs and noninvestigational medicinal products (N-IMPs) must be qualified, able, and willing to follow good manufacturing practice (GMP) requirements. Even those companies involved in direct distribution (couriers) should follow standards such as the good distribution practice (GDP) guidelines of the European Union, highlighted in the “GDP Requirements” box above.
For ensuring that suppliers are reliable, we recommend a three-step qualification of each party. Start with a request-for-information (RFI) approach to obtain business and quality feedback. The next step is a supplier audit, followed by implementing quality and technical agreements in addition to standard business terms and conditions.
Storage capabilities also must be evaluated at investigational sites. During study planning, assess those sites in terms of their respective storage space. For example, it is important to evaluate key cold-chain aspects early on, including whether products must be stored in controlled-temperature areas. If so, validated cold chambers/ refrigerators must be available as a prerequisite. Often this is not the case. So appropriate temperature loggers — even refrigerators on occasion — would need to be distributed alongside the drugs to guarantee environmental monitoring 24 hours/day, 365 days/year.
Managing clinical site logistics is complex, but it becomes even more challenging to support patients in the increasing trend toward direct home delivery for clinical studies. However, some of the same principles used to manage sites can apply to such situations.
Cold-Chain Considerations
To ensure patient safety and uninterrupted dosing schedules throughout each study, drug distribution facilities need to ensure real-time supply chain metrics. Such facilities also must support controlled-temperature storage at different levels such as ambient, controlled ambient, refrigerated, frozen, and deep-frozen conditions.
The cold chain is a critical part of biopharmaceutical logistics. Imperative for ensuring biologic product safety and stability — and therefore product safety — is a correctly managed cold-chain procedure. Also true for commercial medicines, this issue is particularly crucial with clinical-trial materials.
Most of today’s IMPs require temperature control, especially in the realm of oncology and large-molecule research. This not simply a matter of inserting a few gel packs into a case. Biologics must be transported in ambient conditions (typically around 2–8 °C) by making use of tools such as temperature-monitoring devices, temperature-controlled shipping containers, and full track-and-trace technology.
To ensure proper temperature and monitoring, a computerized environmental (temperature and humidity) monitoring system should be used in addition to internal and external security systems. User-friendly Internet- or cloud-based interface systems and real-time data exchange among manufacturer/CMO, third party, and client systems is another key aspect for proper storage practice. Real-time data allow companies to make decisions throughout their development processes, accelerating time to market and reducing overall costs.
Regulation Preparedness
Whatever hurdles may be faced en route — language barriers, environmental changes, or complex import and export procedures — IMPs must finish their journey in the same condition as when they began. This requires a strong understanding of regulatory requirements at both the global and local levels. Logistics managers must account for the impact of their timelines on cold-chain management. This is accomplished through a fully documented quality system, with a change control system and corrective-and-preventive-action (CAPA) plan in place. All outsourced activities must be managed with quality risk management (QRM) in mind. The “GDP Requirements” box goes into more detail (2).
Track and Trace
Arguably one of the most important aspects of storage and distribution is keeping track of products. Fortunately, technical systems and applications in the clinical-trial material supply chain can help manage inventory with full track-and-trace of IMPs and N-IMPs.
Many rules and regulations cover how IMPs should be tracked. For example, the European Commission Director General for Health and Consumers has set clear expectations in the EU-GMP regulations (3). According to chapter 8.24, specific to IMPs, all trial sites should be identified and countries of destination should be indicated. Further, in the case of an IMP for which a marketing authorization has been issued, a contract manufacturer should (in cooperation with the product sponsor) inform the marketing authorization holder of all quality defects that could be related to that authorized medicinal product. Its sponsor should implement a procedure for rapid unblinding of blinded products when necessary for a prompt recall. And the sponsor should ensure that such procedures disclose the identity of blinded products only to the extent that is necessary.
Technical systems are needed to manage inventory of trial drugs in transit and at the manufacturer’s facility, a central depot, local depots, investigational sites, and (ideally) with patients participating in clinical trials. During a recall, products must be immediately quarantined at all storage locations, wherever they can be found, and all involved parties must be informed as a solid recall process is enacted.
When temperature-sensitive drugs are distributed from a central depot to local depots, their temperature and progress must be monitored. When products arrive at their final destination, staff must perform temperature read-outs from embedded data-logger sensors. Drugs can be released for further use only upon successful analysis of those results. The same applies for distribution from local depots to clinical sites or directly to patients. Thus, courier providers must be trained on drug-handling procedures — as must clinical personnel and patients.
Suppliers have developed track-and-trace solutions, mainly interactive response technologies (IRTs) often combined with randomization functionality. However, many such systems do not focus on the complete supply chain — central depot, local depot, courier, broker, site, and patient — and few have full traceability covering what is managed and maintained beyond a central/local depot. For instance, what if a product at a depot was outside its set temperature range for a short period — but in line with stability data? It still could be usable for a clinical trial if no further temperature extensions are documented. But how would all temperature data be mapped?
CMO track-and-trace systems and IRT solutions thus need to be further interfaced to secure end-to-end supply trackability and traceability.
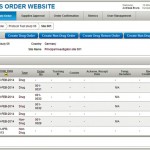
No IRT solution may be in place for open-label trials. And consider what additional clinical trial materials will be needed for each site, such as infusion pumps or specific application materials. Inventory control and track-and-trace tools are still key to ensuring uninterrupted outbound supply, especially for recall situations. Ideally a system should be in place to manage the journey of all products from depot to their site of use. Figure 1 is an example of a specific Internet-based, validated, supplies order module (SOM) for managing such mission-critical processes.
Future Considerations
No one-size-fits-all solution can be applied to drug storage and distribution. What might be essential for one clinical trial could not be the most important consideration for another. However, some universal best practices will make storage and distribution easier to implement: Plan ahead, know your partners, be knowledgeable about the challenges you will face (e.g., the cold chain, local regulations), and leverage available technical tools to the fullest extent possible.
It is our clear expectation that CMOs, CROs, and courier providers play the important role of an industry consultancy. Service providers are engaged in multitudes of storage and distribution projects, including import and export of materials. So they should share their lessons learned in order to drive innovation. Improvements in controlled-shipment boxes, new methods of temperature monitoring, and just-in-time transportation solutions are examples of innovations that outsourcing partners can establish and implement for the biopharmaceutical industry.
The logistics of dealing with effective storage, distribution, and regulatory compliance can be complex and complicated. However, by following established best practices, you’ll ultimately help simplify your drug development journey through the clinical trial process.
References
1 Internal survey and report. PAREXEL International Corp (Waltham, MA) and Industry Standard Research (Cary, NC), 2013.
2 Guidelines of 5 November 2013 on Good Distribution Practice of Medicinal Products for Human Use. Off. J. European Un. 5 November 2013: 343/1–14; http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:C:2013:343:0001:0014:EN:PDF.
3 Chapter 8: Complaints, Quality Defects and Product Recalls. EudraLex: The Rules Governing Medicinal Products in the European Union, Volume 4 — EU Guidelines for Good Manufacturing Practice for Medicinal Products for Human and Veterinary Use. European Commission Health and Consumers Directorate-General: Brussels, Belgium, 17 January 2013; http://ec.europa.eu/health/files/gmp/gmp_chapter8_en.doc.
Jens Mattuschka is vice president, and Vincent Santa-Maria is senior director of clinical logistics services at PAREXEL International Corp., 195 West Street, Waltham, MA 02451; 1-781-487-9900; www.parexel.com.