With one eye on commercialization and the other on monitoring every-day challenges, cell therapy manufacturers are asking critical questions about process efficiency, ensuring quality, and satisfying regulatory demands. In this “virtual” roundtable discussion (participants were asked questions separately), cell therapy industry representatives answer key questions in hopes of broadening understanding about this new class of biopharmaceuticals. Participants in this roundtable are Timothy Fong, PhD (director cell therapy, Becton Dickinson Biosciences), Annemarie Moseley, PhD, MD (CEO, Repair Technologies), Firman Ghouze (director of cell therapy, GE Healthcare), Aby Mathew, PhD (senior vice president and chief technology officer, BioLife Solutions), and Robert Deans (vice president of regenerative medicine at Athersys and ISCT committee chairman).
Processing
BPI: How does the processing of therapeutic cells differ from that for traditional biologics?
Fong: Cells are rather fragile, so techniques used for purifying small molecules or biologics are too harsh, because they are mostly physical methods of isolation with potentially extreme non-physiological conditions. Many cell processing protocols use a combination of traditional cell culture methods and techniques used in peripheral or cord blood banking such as elutriation. When I think about cell therapy processing, I think more about antibody-based separation methods. There are two main types: magnetic-bead–coupled antibody reagents and flow-activated cell sorting (FACS). However, as of today no FACS systems are what I would consider to be completely compliant with current good manufacturing practice (CGMP). So cell processing companies need to jump through some additional hoops in terms of process development and validation to comply with regulatory aspects of cell CGMP processing.
Moseley: If the cells are frozen, they need special handling, and you need to pay attention to the timing of therapies. Under “biotechnology conditions” cells cannot survive or they are modified. Cell therapy processing reactors are different, and there are no ultracentrifuges. Currently there is not even a good way to reduce volume from a large cell collection. So there is a lot of room for manufacturing improvements — all likely to come after the first product is approved.
Ghouze: Some manufacturers use tangential flow filtration (TFF), in which the cells aren’t rammed against a filter membrane. Many facilities that develop cells either have discrete closed systems to process these cells, or they have a large CGMP-type laboratory that works with cells.
Fong: One of the current major needs in processing and isolating cells in general is the development of better closed systems in which we can isolate, grow, activate, and expand them. The technology is emerging, but we don’t have a lot of choices in hand to facilitate that.
Moseley: Manufacturing is still very people-dependent. It requires a lot of oversight and very intense manipulation by personnel, as opposed to robotics and automation in biopharmaceutical processing. Scale-up and logistics are still in their infancy. It’s much like the antibody industry, in which initially no one could do it, so companies had to hire contractors. Now everyone is making antibodies in-house. I think that is eventually where we are going to see this field moving.
BPI: What equipment is used to manufacture cell therapies?
Moseley: Most companies have customized processes, so there are no standardized bioreactors, for example. Cells used in antibody production have been manipulated to the point where they can be in suspension, but most adult stem cells like being attached to a surface. Designs using many tubes or beads have been tried, but right now there are only a few containers that have a lot of surface area. The primary of those are Cell Factories (Nunc, ThermoScientific, www.nuncbrand.com). They resemble a lot of tissue flasks glued together. Those designs have not addressed scale-up. They are simple because so far there hasn’t been much demand for them. As demand increases, the industry will need a “cell reactor.” But right now, there aren’t enough companies with products in the intermediate phases, so they are having to adapt their collection systems and centrifugation steps.
BPI: How will scale-up become an issue as products progress to commercialization?
Ghouze: Getting cells of the required quality in a scalable manner will be a challenge. Companies can successfully process them at a scale for small clinical studies (trials with 10–20 patients). But if some of those cell therapies progress in the way industry hopes, and if clinical trials progress well, then companies will need scalable solutions from a CGMP facility to enable really widespread distribution.
Moseley: Each Cell Factory system has a few liters of volume media in it that must be centrifuged to collect the cells, which is a problem at scale-up. Currently there are no large-scale systems for handling that much media. So researchers have been trying to figure out different ways to speed up the process of centrifugation before cells are diluted in freezing media. All the centrifuge systems used to collect the antibodies off of the reactors are way too harsh for the cells because antibodies are so much smaller. The process of getting massive volumes of cells and combining them is not automated, and companies have been trying to figure out ways to do that efficiently. There are some real opportunities for process development, automation, and new devices. It’s just a question of what is going to trigger that work. A lot will depend on market need and whether many companies will be doing that part of the process themselves or whether it will be done through a contract services provider.
REGULATIONS AND SAFETY
BPI: What is your understanding of FDA requirements for assays and testing?
Moseley: The FDA requires the same global release criteria in terms of sterility, potency identity, and so forth as for antibodies. Assays to date have been based on the identity of the cells as stem cells, and potency assays have varied based on the indication and whether a company chooses to focus on indication potency or potency as to “stem cellness.” The same types of toxicity testing apply, although biodistribution is different and duration of the studies has been longer in some cases, making preclinical studies more costly.
BPI: What is your understanding about guidelines for operator safety?
Fong: Peripheral and cord blood banks primarily use closed cell-processing systems. A Class 10,000 room is perfectly acceptable for those types of systems. Other processes such as FACS cell isolation are not closed systems. My current understanding is that a Class 10,000 room or equivalent is probably required in addition to some
sort of biosafety cabinet for flow instruments. Obviously, a major concern is operator safety because flow sorters are not closed systems, and most of them have some level of aerosolization. As far as handling of large numbers of cells before, during, and after cell manipulation, a lot of the systems that cell therapy developers are using today have been co-opted from the blood banking industry. So suppliers need to think how they can develop more specific closed systems for all the different types of cells — stem cells, adherent cells, suspension cells — that companies will be wanting to grow for future cell therapies.
A lot of developers have become very familiar with the guidance for cord blood banking, tissue processing guidelines, and biologics manufacturing guidelines, particularly when it concerns manufacturing reagents. Take antibody-based separation methods, for example. If you look through the FDA guidelines for cell therapy, it refers back to manufacturing guidelines for therapeutic monoclonal antibodies. So in a sense, even though your antibody reagent is really part of your process for isolating your cells, manufacturing to guidelines is essentially equivalent to a therapeutical monoclonal antibody. Having said that, I believe that most regulatory agencies are flexible, and they’re looking at each IND application and cell manufacturing process case by case to determine whether the level of CGMP compliance is acceptable for that particular application. As far as I can tell, in general, FDA and EMA are trying to follow similar guidelines. One issue unique to Europe is that in addition to EMA regulations, you have national and regional regulations that can add another layer of complexity.
BPI: Cryopreservation is an important processing step for some cell therapies. What techniques are currently used?
Mathew: Techniques are usually separated between the standard cryopreservation methods (used by most) of traditional ice management home-brew freeze cocktails or the newer class of intracellular like complex formulations; and then to a lesser degree vitrification. Certainly, controlled-rate freezers have allowed programming and greater manipulation of freezing rates throughout a cryopreservation protocol, but even isopropanol freezing containers have made it easier for folks to have more consistency in their cryopreservation protocol.
BPI: What tests are used to ensure cells are viable after cryopreservation?
Mathew: All biologics are normally maintained under normothermic conditions either within the body or as part of cell culture conditions. However, once cells are removed from normothermic conditions, changes occur in their metabolism and cellular integrity. If these changes are reversible, then cells can recover appropriately upon return to normal conditions. If the stresses of these changes build up too much, the cell is negatively influenced to undergo active pathways of breakdown (such as apoptosis) or passive pathways of breakdown (such as necrosis).
Tests used to ensure viability (and/or functionality) are varied and debatable regarding appropriateness. For cell therapy, viability is often assessed immediately postthaw by simple live/dead assays that may not indicate the true, long-term viability of the cells due to the phenomenon of preservation-induced, delayed-onset cell death.
During cell therapy product characterization and manufacture, it would behoove a manufacturer to validate the efficacy of its preservation methods with multiple viability, potency/functionality, and stability assays. For broad application to many cell types, you can use tests such as live/dead assays that can be assessed with a fluorescent plate reader or flow cytometer. Metabolic assays and membrane integrity tests are another method of assessing cell health. Furthermore, analysis of the “-omics” (e.g., genomics, proteomics, metabolomics) allows for in-depth characterization of a cell product. And these assessments should be performed on the cell product at multiple stages in the stability intervals to better understand the limitations of the overall system of manufacturing, banking, and/or transport, and clinical delivery application. An optimized biopreservation system would allow clinical and commercial development of cell and tissue products with the greatest clinical efficacy, lowest manufacturing costs, and greatest stability to enable worldwide distribution.
The biggest disparity is that there is the “academic/basic science” perspective to cryopreservation and a “process development” view. Academically, each cell/tissue type has its own characteristics of water content, membrane permeability, size, sensitivity to stress, and so forth. However, from a process perspective you do not want to have to use a custom process and custom solution for each cell type. A cell therapy company that invests a lot into its specific cells (such as custom growth media) may be okay with a custom freeze process if all it is working on is that cell type. But if you are a cell supplier, or a pharmaceutical toxicity group that might be concurrently working on CHO cells, hepatocytes, or iPS cardiomyocytes, then no one will want to have to use a separate cryopreservation process for each of these cell models. Cell therapy groups do not want to invest more time and resources than needed into optimizing freeze media or cooling rates, so cryopreservation methods that support a streamlined, consistent, and effective process will enable them to achieve their goals sooner rather than later.
BPI: Are there concerns about safety and quality?
Moseley: Preclinical and safety issues mostly refer to embryonic stem cells. What you need to do to demonstrate safety for the adult stem cells has become almost routine now with the FDA because probably up to 10 companies or more and many protocols (over 50 already) have gone through the FDA on this area. So that is not so much an issue, but every embryonic program will have its own issues and programs.
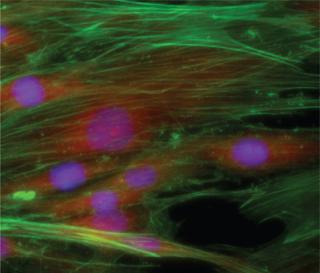
Fong: One major misconception is that cell therapy is a brand new field. If you define cell therapy as using cells to try to treat a medical condition, the actual history goes back over 100 years with blood transfusions and almost 60 years with bone marrow transplant. However, what is new is the type of cells and the sources of cells that we are using. New developments are our greater understanding of stem cells and mature cells such as T cells and other lymphocyte populations. We have a better understanding of their phenotypes, a better methodology of isolating them to greater homogeneity, and a greater understanding of how cells act in normal physiology as well as in disease. So now we can begin to manipulate them and use them in our favor to treat disease. That goes hand in hand with improvements in cell characterization and isolation.
Ghouze: Because bone marrow transplantation has been around for a long time, cell therapies based on bone marrow cells have quite a robust quality control (QC) process. There are various techniques people can use to define whether the cells used with engraftment have a high likelihood of success, for example. There is a drive toward standardization, for QC technologies to define what makes a cell effective and safe. The industry is currently moving in that direction, but there is still some ways to go in that area. The mechanism is poorly understood in some instances. Having said that, people will use existing technologies such as flow cytometry, but it must be scalable.
Robert Deans: There will always be different perspectives on safety. With the development of new and more sensitive safety testing, tools, and procedures, there is always going to be a need to further educate and reevaluate. But I don’t see the adult cell therapeutic space as being considered highly risky at this point. Regulatory agencies are encouraging development and supporting trials in this area; and there has
been a very good safety track record, especially in the case of mesenchymal stem cells (MSCs). I think there are now more than 5,000 patients who have been treated with MSCs. So I don’t see it as a safety issue; I see it as a matter of education.
Potency assays are a very hot topic. This relates to how cells are characterized either phenotypically or functionally, which in turn relates to their biological performance. Part of the issue also involves the intellectual property that protects many cell therapeutics. Investment and development in this space is also going to be driven around intellectual property boundaries. We have an insufficient hold on quantitatively measuring potency and then comparing potency among alternative but related cell types. That is a very big area for scientific and technology development, and it’s one of the topics that is very important for open debate so that potential financial investors have an opportunity to hear scientists make an opinion on assays that they trust and information they would require before making a decision.
Author Details
Maribel Rios is managing editor of BioProcess International, 1-646-957-8884, mrios@bioprocessintl.com.