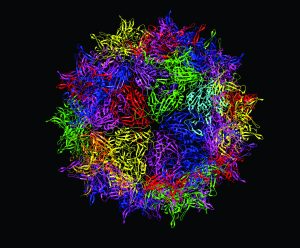
A ribbon diagram representing the capsid of adenoassociated virus serotype 2 (AAV2, one fivefold-symmetry axis shown at center) https://www.wikipedia.org
Gene therapies based on adenoassociated virus (AAV) vectors hold promise for treating myriad conditions. Immunogenicity remains a challenge for such products, however. With support from PerkinElmer, Roland W. Herzog (professor of pediatrics and Riley Children’s Foundation professor of immunology at the Indiana University School of Medicine) joined Nagendra Venkata Chemuturi (scientific director of global research for drug metabolism and pharmacokinetics, DMPK, at Takeda Pharmaceuticals) to deliver a BPI “Ask the Expert” presentation exploring strategies for minimizing immune responses to AAV-based products. Herzog described emerging research on the role of innate immune signaling in adaptive immune responses to AAV. Chemuturi highlighted the increasing importance of clinical pharmacological tools for evaluating AAV biodistribution.
Herzog’s Presentation
Clinical Observations: AAV-based products have raised immunogenicity concerns during clinical evaluation. Because AAV infection occurs naturally, some trial subjects already have neutralizing antibodies (nAbs) against the virus before treatment, preventing gene transfer. AAV capsid proteins also are known to activate CD8+ T cells when administered to liver and muscle cells. At high doses, such products that are formulated for systemic delivery can activate the complement system — including proteins that require mediation from antibodies and others that bind directly to capsid proteins to induce opsonization. In addition to those challenges, clinical trials for AAV-based products have documented immunity-mediated hepatotoxicity and tissue inflammation, especially in sensitive regions such as ocular tissues.
New Approaches: Although administering immunity-modulating agents during a gene-therapy regimen can diminish T-cell and complement activation and facilitate target-gene transfer, clinical-trial subjects have responded inconsistently to such interventions. Many gene-therapy developers are redesigning viral vectors to minimize their immunogenicity, and a promising way to do so is to disrupt the activity of toll-like receptor 9 (TLR9) proteins that drive some immune responses to AAV. TLR9s are expressed on many immune cells, including plasmacytoid dendritic cells (pDCs), which play a key role in linking innate and adaptive immune responses. When TLR9s detect AAVs, pDCs produce type-one interferon (IFN-1), which binds with receptors on conventional DCs (cDCs) that release other T-cell activating factors.
Given that pathway, researchers are engineering vectors with genomes bearing few unmethylated CpG oligonucleotides, which are strong activators of TLR9. Clinical evidence now supports that approach. In trials for AAV-based products for hemophilia, candidate therapies with few CpG motifs achieved more sustained expression of target genes in patient cells than did products with genomes bearing many such nucleotides. Using mouse and macaque models, Herzog’s team has shown that applying CpG-depleted vectors can diminish T-cell activation — but that doing so cannot be counted on to reduce antibody formation against AAV capsid proteins.
Herzog also described a multilaboratory study that evaluated an CpG-depleted AAV3 vector for expression of human coagulation factor IX in three nonhuman primates. Low vector doses achieved high factor IX activity in two subjects; the third showed no such increases because it had developed nAbs to the AAV capsid. No subjects showed CD8+ T-cell activity in response to capsid proteins, elevated liver enzymes emblematic of tissue damage, or antibodies against factor IX. Such findings, Herzog explained, confirm the merit of a CpG-depletion approach, and researchers are beginning to find ways to mitigate the limiting effects of AAV nAbs.
The Complexity of Immunogenicity: Herzog noted that some CD8+ T-cell responses to AAVs occur independently of TLR9 detection. His team recently determined that tissue damage related to high doses and specific routes of administration can release IFN-1, double-stranded RNA, and other molecules that initiate cDC cascades.
Some innate-immunity signals can spur on adaptive responses to transgenes. In another set of studies, Herzog’s team coadministered AAV vectors for factor IX and different TLR activators into the skeletal muscle tissue of mice, then tested the subjects for factor IX activity. Applications of TLRs 2, 4, and 7 initiated no immune responses to factor IX, but using TLR9 prompted significant production of antibodies against the factor. That response traced back to monocyte-derived DCs, and such responses can be curbed by modulating regulatory T-cell activity.
CpG-depleted AAV vectors hold much promise in mitigating immunogenicity concerns. However, researchers also must investigate dosing and administration further to modulate other immune pathways that diminish AAV gene transfer, including those that are initiated by innate immune signals and then executed by antibodies.
Chemuturi’s Presentation
Advancing gene-therapy development will require consideration not only of AAV immunogenicity, but also of biodistribution — distribution, persistence, and clearance of a product from target and nontarget tissues. Many of the absorption, distribution, metabolism, and excretion (ADME) principles that were developed for evaluation of small-molecule drugs and conventional biologics do not apply to viral gene therapies. Thus, much work lies ahead for pharmacologists in elucidating AAV’s disposition. DMPK activities will inform capsid and promoter selection, clinical-trial design, and product labeling.
Biodistribution: Viral gene therapies require more extensive analysis than what can be achieved by plasma concentration-time studies and other standard distribution assessments. Because vectors deliver functional genes, pharmacologists must investigate whether product binding with nontarget cells (e.g., gametes) could induce adverse effects. When developing biodistribution assays, analysts should focus on a vector’s capsid rather than its genome because the former determines which cells a virus can infect. Tropism also influences how a vector is distributed differentially to organs and tissues.
Route of drug-product administration merits special consideration because it can influence a product’s biodistribution. When feasible, local administration is preferable over systemic delivery for delivering high vector concentrations to the site of action while sparing off-target tissues from undue exposure. Systemically administered viral vectors often concentrate in the liver and spleen, but locally administered therapies can drain into proximal tissues and systems.
Regarding preclinical testing, Chemuturi advised implementing several time points after the expected time of peak product detection. It can be difficult to determine when AAV-based products indeed have cleared.
Shedding Studies: AAV-based candidates must undergo testing for potential shedding of intact virions to caregivers and clinicians. Analysts also must determine environmental risks associated with releasing new genetically engineered viral vectors. During such studies, pharmacologists should consider the parental/wild type virus’s natural route of infection, infectivity, pathogenicity, replication competence, propensity for inadvertent transmission, and integration capability. Shedding studies also should account for preexisting immunity among patient and nonpatient populations.
Although such studies typically are performed using polymerase chain reaction (PCR) assays, analysts can use several sample types, including saliva, nasal and pharyngeal secretions, tears, feces, and urine. A product’s route of administration will influence its shedding profile, as will concomitantly administered drugs. Data from shedding studies ultimately help to develop instructions for handling of patient secretions and excreta.
Dose Selection: Because viral gene therapies behave differently from other modalities, especially regarding species specificity and immunogenicity, pharmacologists cannot rely only on allometric scaling to evaluate first-in-human (FiH) dose requirements. Analysts should consider all preclinical data to determine a FiH dose and support selection of a particular route of administration and application device.
When a therapy will be delivered to specialized tissues, careful attention should be given to organ/tissue-specific parameters (e.g., differences in vitreous humor volumes between nonhuman and human subjects’ eyes). Regulatory agencies permit gene-therapy developers to use clinical data obtained for similar products to support FiH dose specifications, even if those comparators used different routes of administration. After early phase trials, developers can adjust dosing based on efficacy and safety findings.
Spurring on Gene-Therapy Development: Several pharmacological challenges hamper the clinical development of AAV-based products, Chemuturi explained. Some therapies require invasive administration, and dosing often cannot be adjusted for different patient populations. After administration, a therapy’s effects can be difficult to abrogate, and immunogenicity can limit the efficacy of subsequent doses. Developers remain uncertain about the durability of gene-therapy outcomes.
However, opportunities abound for improving gene-therapy DMPK assessment. In silico modeling tools and quantitative systems pharmacology (QSP) approaches are improving prediction of therapy biodistribution, immunogenicity, and durability. Chemuturi emphasized that because gene therapies continue to evolve, pharmacologists need to tailor DMPK studies to a product’s serotype, route of administration, and indication.
Questions and Answers
What factors raise the most pressing immunogenicity concerns? Several factors are implicated in viral-vector immunogenicity. Serotype and capsid tropism are important considerations, but vector dosing can influence how many capsid proteins and how much viral DNA the innate immune system can recognize — and that detection capability can differ by tissue type.
What immunomodulating regimens are being evaluated alongside gene therapies during clinical trials? Steroids have been applied in several trials to suppress a product’s inflammatory effects at the time of gene transfer. Emerging protocols combine transient immune suppression with gene transfer to minimize immunogenicity and toxicity events.
Is it possible to eliminate a vector’s immunogenicity entirely? Although that outcome is impossible, researchers can develop modalities that minimize immune responses of concern such that immunomodulating therapies need not be coadministered to enable sufficient gene transfer.
Brian Gazaille is associate editor of BioProcess International; brian.gazaille@informa.com. Roland W. Herzog, PhD, is professor of pediatrics and Riley Children’s Foundation professor of immunology at the Indiana University School of Medicine, 340 West 10th Street, Fairbanks Hall, Suite 6200, Indianapolis, IN 46202; 317-274-8157. Nagendra Venkata Chemuturi is scientific director of global research for DMPK at Takeda Pharmaceuticals, 35 Landsdowne Street, Cambridge, MA 02139; 617-679-7000.
These presentations were made possible with support from PerkinElmer. For inquiries, please contact senior strategy leader in pharmaceutical development Anis H. Khimani, 68 Elm Street, Hopkinton, MA 01748; anis.khimani@perkinelmer.com; 774-278-2648; https://www.perkinelmer.com.
