Ebola: Biotech Goes on Counterattack
by Cheryl Scott
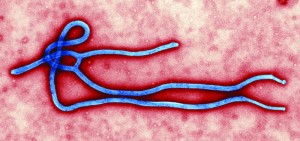
It seems that every year brings a new virus or bacterium to the forefront of the public’s limited attention for infectious disease research. Sometimes it’s a newly identified pathogen such as the severe acute respiratory syndrome (SARS) virus. Often, however, it’s a new strain of influenza or other species — as is the case with this year’s growing focus on the Ebola virus. As recently as March 2014, Reuters was reporting on “scant funds and rare outbreaks” that led to a “slim” drug pipeline. One of the most deadly viruses known to humans, Ebola was the subject of some government research due to fears of its potential use as a bioweapon. But few companies were involved because the disease’s rarity offered little potential return on investment.
A new strain was identified in April as being responsible for dozens of deaths in Guinea, and then it began to spread — most likely due to the less than stellar capabilities of west African rural healthcare. The virus is zoonotic in nature, infecting both humans and animals, which makes outbreaks most likely to occur in areas where containment is problematic. Before long, aid workers from developed nations were getting sic . Once considered a quintessential “niche disease,” over the past six months Ebola has become the most talked- about pathogen on cable news.
Not surprisingly, all that increasing interest has brought some funding windfalls to those companies that have been working to develop drugs, diagnostics, and vaccines aimed at this type of infection. The much- needed cash influx is keeping some afloat while others are even restarting previously abandoned programs. Meanwhile, the media ask, “Why are these drugs being kept from the poor people in Africa who need them?” Of course, that leads many in the industry to shake their heads in frustration over the lack of public understanding when it comes to drug development, manufacturing, and approval. The World Health Organization is careful to limit use of untested drugs to the best available candidates.
To complicate matters, Ebola’s close cousin the Marburg virus is now circulating in the same African countries. During a 2004–2005 outbreak, >90% of Marburg patients died; >1,400 people in West Africa have died of Ebola this year. Progress is being made, though, and many companies are going after both diseases simultaneously:
- GlaxoSmithKline bought Swiss company Okairos in 2013 and is now putting development of the Ebola vaccine program that came with it into high gear — shooting for a 2015 launch.
- Mapp Biopharmaceutical’s and Kentucky Bioprocessing’s tobacco-produced experimental ZMapp monoclonal antibody (MAb) was given to several stricken westerners. But scant supplies of it have since been used up.
- Previously subject to a clinical hold by the US Food and Drug Administration (FDA), Tekmira Pharmaceuticals’ experimental RNA-interference therapeutic has been approved for emergency use (perhaps due to depletion of ZMapp supplies).
- The US National Institute of Allergy and Infectious Diseases (NIAID) has given drug developer BioCryst Pharmaceuticals US$6 .5 million in grants to test an experimental antiviral drug to treat Ebola.
- Johnson & Johnson has teamed up with Danish biotech Bavarian Nordic and NIAID to create a combination vaccine, with clinical trials planned for early 2015.
- The U .S . Food and Drug Administration (FDA) has okayed human clinical trials of NewLink Genetics’s experimental Ebola vaccine, which was licensed from Canadian government researchers.
- Partners Inovio Pharmaceuticals and GeneOne Life Science plan to assess their experimental vaccine in human clinical trials in the first half of 2015.
- Troubled Hemispherx Biopharma is forming five new collaborations to accelerate testing on its Ebola candidates.
- Scientists at Siriraj Hospital in Thailand claim to have discovered an antibody that’s small enough to get into infected cells and demolish Ebola proteins.
- Publicly traded companies such as Chimerix and Immunovaccine have seen their share prices spike on announcements of progress for their Ebola products.
- Other companies involved in Ebola developments include Profectus Biosciences, Sarepta Therapeutics, NanoViricides, Defyrus, Vaxart, Inovio Pharmaceuticals, and Corgenix.
- Three US Centers for Innovation in Advanced Development and Manufacturing — run by Texas A&M University, Novartis, and Emergent Biosolutions — are being made ready to manufacture treatments and/or vaccines if that becomes necessary.
Meanwhile (and perhaps inevitably), as legitimate sponsors continue their hard work, the FDA is reporting that Ebola “treatments” and “cures” are already being sold online by less trustworthy companies. The agency is doing its best to warn consumers away from those fraudulant products. And it’s cracking down on snake-oil salesmen marketing essential oils for such purposes.
Two ISPE Programs Move Forward
This past summer, the International Society for Pharmaceutical Engineering (ISPE) released a preview of its Drug Shortages Prevention Plan.
 This plan is intended to help the industry prevent drug shortages and maintain a robust and reliable supply of medications to patients world-wide. It was developed by ISPE members to describes how industry can discover the root causes of drug shortage, then create and sustain organizational cultures supported by leadership, business processes, and quality systems to ensure a robust, resilient, and reliable supply to patients worldwide. An introductory summary available online (www .ispe .org/drug- shortages-initiative/plan-intro-summary.pdf.) provides a first look. Part of the ISPE’s overall Drug Shortages Initiative, the plan has been reviewed by European regulators, with further regulatory review anticipated.
This plan is intended to help the industry prevent drug shortages and maintain a robust and reliable supply of medications to patients world-wide. It was developed by ISPE members to describes how industry can discover the root causes of drug shortage, then create and sustain organizational cultures supported by leadership, business processes, and quality systems to ensure a robust, resilient, and reliable supply to patients worldwide. An introductory summary available online (www .ispe .org/drug- shortages-initiative/plan-intro-summary.pdf.) provides a first look. Part of the ISPE’s overall Drug Shortages Initiative, the plan has been reviewed by European regulators, with further regulatory review anticipated.
Built upon results of a 2013 study on drug shortages, the plan is organized around a “six-dimension” framework: corporate quality culture, robust quality systems, metrics, business continuity planning, communication with authorities, and building capabilities. The task team engaged with leaders from more than 30 big pharmas and gathered stakeholder input from hundreds of industry professionals at ISPE conferences and workshops.
“Quality systems can be effective only where there is a strong emphasis on a ‘corporate quality culture’ throughout an organization,” says Francois Sallans (VP and CQO at Johnson & Johnson), chair of the task team.
On a related matter, the ISPE Quality Metrics Pilot Program has confirmed participation of 12 companies and 32 sites — as recruitment continues. So far, these companies represent generic, innovator, over-the-counter, contract manufacturing, and analytical companies involved in a range of products.
A team meeting in July led to establishment of forums at which participating companies can influence the pilot program’s outcome and opportunities for participants to develop insights into the quality performance of their own sites. “Wave 1” participating companies will provide up to 12 months of historic and three months of current data as Wave 1 of the Program. Based more on current data collection and analysis, “Wave 2” will expand the number of participants; assess a metric set; include input from subteams working on leading quality indicators, quality culture, and process capabilities; and may cooperate with other groups and associations. The objective is to provide experiential input on development and use of quality metrics for the benefit of both industry and regulators.
To participate, contact PQLI@ispe.org or McKinsey & Company at ispe_pilot@mckinsey.com.
Delivering Biologics Anthrax-Style
A team of MIT researchers has engaged the anthrax toxin as a potential delivery system for cancer drugs. These scientists used a disarmed version to deliver two antibody-scaffold fragments into cancer cells — the first successful such delivery. Many antibody drugs target cell-surface receptors, but it can be difficult to get therapeutic proteins inside cells. For decades, biochemists have tried to understand how anthrax toxins get into cells, with some people exploring its potential as a vaccine. The three-part toxin includes one protein that binds to specific receptors on most mammalian cells. That creates a doorway for two toxic proteins to get inside, where they can disrupt cellular processes and cause cell death. Replacing those dangerous proteins with therapeutic ones is the basis of the MIT work.
“Delivery of Antibody Mimics into Mammalian Cells via Anthrax Toxin Protective Antigen” (by Xiaoli Liao, Amy E . Rabideau, and Bradley L . Pentelute) went online 22 September 2014 for the ChemBioChem journal: http:// onlinelibrary.wiley.com/doi/10.1002/cbic.201402290/full.